MSS08: NATIONWIDE BLUNT CEREBROVASCULAR INJURY OUTCOMES IN THE PEDIATRIC POPULATION: BIG PROBLEMS IN LITTLE PATIENTS
Christoper W Marenco, MD1, Woo Do, MD1, Daniel Lammers, MD1, Matthew Eckert, MD1, Carly Eckert, MD1, Denis Bensard, MD2, Matthew J Martin, MD1; 1Madigan Army Medical Center, 2Children's Hospital Colorado
Objectives: Blunt cerebrovascular injury (BCVI) is an uncommon but potentially devastating injury with consequences including stroke and death. The epidemiology, outcomes, and screening criteria are well described in adults, but existing data in the pediatric population is limited to small single or multi-center series. The objective of this study was to characterize pediatric BCVIs in a large nationwide sample with a focus on epidemiology, outcomes, associated injury patterns, and risk factors.
Methods: Retrospective review of the national Kids' Inpatient Database (KID) for all blunt trauma patients with ICD-9 diagnosis codes for BCVI from 2000-2012. Patients were stratified by age and vessel injured. The primary outcomes of the study were stroke and mortality. Patient demographics, injury severity, hospital region/size, and previously described risk factors for BCVI were also compared between groups.
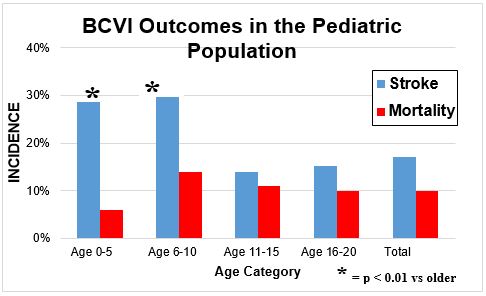
Results: We identified 1182 cases of BCVI from 577,308 admissions for blunt trauma, yielding an overall incidence of 0.21%. Patients were predominately male (69%) with mean age 15 ±5 years. Injuries included 700 (59%) carotid, 155 (13%) vertebral, and 327 (28%) unspecified cervical vascular injuries. Multiple vessels were injured in 15%. Overall mortality rate was 10% and did not differ between age groups (p=0.4). However, the associated stroke rate was significantly greater in the younger age groups (see Figure, 29% for ages 0-10 vs. 15% for ages 11-20, p<0.01). Older children were more likely to be severely injured (ISS>15, 53% v. 36%, p<0.01), while younger children frequently lacked associated severe injury patterns. Only 4 of 7 commonly utilized BCVI risk factors were significant in children: C1-3 spine fractures (p<0.001), C4-7 spine fractures (p=0.012), basilar skull fractures (p=0.040), and clavicular fractures (p=0.001). However, when stratified for type of vessel and age category, none of those risk factors were significantly associated with BCVI in the younger age group (age 0-10). Hospital-level factors demonstrated no significant difference in stroke or mortality rates based on hospital size or for freestanding children’s hospitals.
Conclusion: This represents the first nationwide assessment of BCVI in the pediatric population. Pediatric BCVIs carry a considerable associated mortality (10%) and stroke rate (17%). Although mortality was similar between age groups, stroke occurred twice as frequently in patients under 10 years of age. Importantly, the commonly utilized BCVI screening criteria were variably useful for all pediatric patients, and were not useful for the younger cohort of age less than 10 years. No outcome differences were noted between pediatric and adult centers.