MSS17: PORTABLE THERMAL IMAGING TECHNOLOGY TO EVALUATE TOURNIQUET EFFICACY IN A FIELD SETTING
Beau J Prey, MD; Andrew D Francis, MD; James M Williams, MD; Hannah M Palmerton, MD; Daniel Lammers, MD; Michael Lallemand, MD; John McClellan; Jason R Bingham, MD; Madigan Army Medical Center
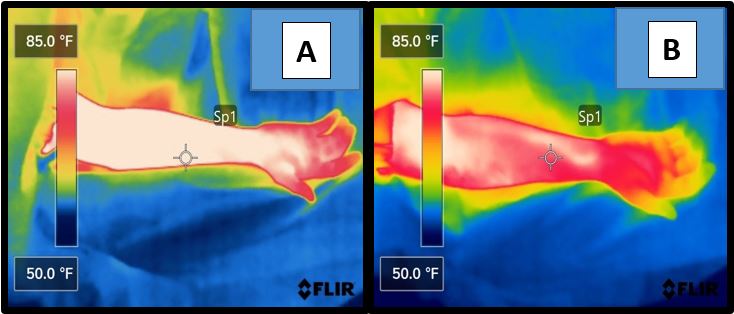
Figure 1. Thermal images of upper extremities in the field care setting prior to tourniquet tightening (A) and after tourniquet vascular occlusion (B).
Objective: Appropriate tourniquet use remains a critical component for hemorrhage control in extremity trauma. Identification of ineffective placement can be challenging, particularly during patient transport. This study sought to evaluate the use of a handheld thermal imaging device for assessing extremity perfusion and adequacy of tourniquet placement based on thermal imaging patterns in healthy human volunteers.
Methods: The FLIR E4 portable thermal imager was utilized under both a controlled intraoperative setting (Phase 1; n=22) and a simulated field care setting (Phase 2; n=26). A series of before and after photos were taken and evaluated by untrained, blinded personnel (n=53) to identify changes in thermal patterns associated with tourniquet vascular occlusion. Mann Whitney U testing was performed to evaluate for differences between patients, and independent t-tests were performed to evaluate test scores.
Results: The median arm temperatures in Phase 1 and Phase 2 were 91.5oF and 86.4oF and 88.6oF (-3.83% change) and 83.1oF (-3.82% change) respectively following tourniquet placement. Baseline thermal imaging characteristics were similar for all participants in both phases. Qualitative thermal image analysis showed clearly visible perfusion differences in both phases. Evaluators were able to correctly identify appropriately placed tourniquets based on thermal imaging patterns with 93% accuracy (87% Phase 1 vs 97% Phase 2; p < 0.01). Differences in age (p = .94) and gender (p = .35) were not factors in the ability to correctly identify tourniquet placement.
Conclusion: Thermal imaging represents a portable adjunct capable of evaluating perfusion and adequacy of tourniquet placement in clinical and field care scenarios. The rapidly accessible and noninvasive nature of this technology may allow for broader clinical applications, however, further investigation should be sought.